Introduction
With the evolution of mankind, the incidence, extent and nature of trauma has undergone radical change. Wars and assault are older than recorded history and maxillofacial trauma has indeed been a major consequence. About 42% of all the injuries affect the craniofacial complex, of which 74% victims are male and 26% are female; 57% of these involve the mandible while 26% involve the midface, 13% affected both the midface as well as the mandible[3],[4].
Around the year 460 BC Hippocrates had described the treatment of fracture of the mandible as, “If the teeth at the wound be distorted and loosened when the bone is adjusted, they should be connected together, not only two but more of them, with a gold thread if possible, but otherwise with a linen thread, until the bone be consolidated”[1].From the year 25 BC to the 11th century AD noted surgeons and writers such as Sushruta, Celsus and Avicenna described the conservative means of treating jaw fractures[1]. In 1492 AD Salicetti advised wiring of one jaw to the other to treat fractures as “….this done, tie the teeth of the uninjured jaw to the teeth of the injured jaw in this way[1].
Angle in 1890 published his technique for control of jaw fractures using modified orthodontic bands, threaded arch bars and screw expansion devices for precise restoration of the teeth and fragments[1],[2]. Oliver (1910) used wire ligatures with a loop to immobilize the jaws, this technique was improved upon by Eby (1920) and Ivy (1922)[1]. Since then numerous methods for instituting MMF have evolved over the ages with newer materials and newer techniques ranging from gold wires tied around teeth to nylon threads, stainless steel wire, various type of splints, eyelets, different forms of arch bars, vaccum formed splints, pearl steel wires, button wiring, bonded brackets, self tapping screws to self drilling transalveolar screws and so on[3]. In the year 1989, transalveolar screws were introduced as a new hardware for maxillomandibular fixation. This method was developed with the main aim to lower the risk of the operator while treating Human Immunodeficiency Virus [HIV] positive patients[5]. Since then these have been put to use for various indications of MMF.
Materials & Methods
In the patients, 2.0 mm diameter, 12 mm long transalveolar self-tapping titanium screws manufactured and marketed by M/s Orthomax, India were used (Figure 1). These screws were placed in maxilla and mandible, two to three screws per arch, strategically so as to avoid root apices or neurovascular bundle, the ideal sites being supero-medial to the maxillary canine and infero-medial to the mandibular canine. After injecting 2% lignocaine with 1:200000 adrenaline by local infiltration in the maxilla and a bilateral inferior alveolar nerve block in the mandible, 1.5 mm diameter drill holes were made transmucosally- not requiring a gingival incision. Each screw was inserted till its head snugly fitted against the buccal mucosa. Once the screws were secured MMF was accomplished by passing 24 Standard Wire Gauge (S.W.G.), soft, stainless steel, pre stretched wires through the slots/ holes on the heads of the screws vertically.
 | Fig 1: Armamentarium Transalveolar Screws (A: Mouth Mirror, B: Tweezer, C: Double Ended Probe, D: Molt’s Periosteal Elevator, E: Universal Screw Driver 2.0 Mm, F: Self Holding Screw Driver 2.5 Mm, G: Needle Holder 6 Inches, H: 24 Gauge Wire, I : Wire Cutt
 |
Results
The mean time for application was23.5 min (standard deviation = 17.8 min) ranging from of 20 to 30 min. The ease of application for the MMF apparatus was graded as “Easy / Moderate / Difficult”, by the operator. It was graded as “Easy” for 8 out of 10 patients and “Moderate” for the other 2 patients. The time taken for removal was 15.5 min (standard deviation = 3.7 min) with a range of 10 to 20 min. The ease of removal for the MMF apparatus was graded as “Easy” for 8 out of 10 patients and “Moderate” for the other 2 patients. The mean duration of MMF was 28 days (standard deviation = 4.7 days) with a range of 20 to 38 days. Stability on removal of the MMF apparatus was marked as “Stable / Unstable” by the operator. 5 out of 10 patients had stable MMF apparatus on release whereas the other 5 were unstable. The stability of fixation on release was marked as “Stable / Unstable”. It was found to be stable in 8 out of the 10 patients whereas 2 had an unstable fixation. The breach of glove barrier was examined at the time of application of the MMF apparatus and was marked as “Positive / Negative”. No perforations were detected after application of the MMF apparatus but at the time of removal of apparatus7 of the 10 removals resulted in no perforations, while in the other 3 procedures, perforations were present. The level of patient comfort was graded by the patient as “Good / Moderate / Difficult” based on his experience. 3 of the 10 patients graded their treatment as “Good”, while 7 graded it as “Moderate”. The mean cost was INR 864.80 (Standard Deviation = INR 135.70) with a range of INR 803 to 1206. Loosening of the MMF apparatus was evaluated throughout the period of MMF and was marked as “Positive” if loose and as “Negative” if stable. 5 of the 10 patients had a loosening of apparatus, while it was as firm as on application in the other 5 patients.
Discussion
The transalveolar screws were developed for decreasing the risk of exposure of the maxillofacial surgeon to needlestick injuries while treating HIV positive trauma patients. Various authors have undertaken studies on a varying number of patients to evaluate the efficacy of these transalveolar screws. The patients in our study were selected serially from the out patient department (O.P.D.) of Oral and Maxillofacial Surgery (OMFS), MM College of Dental Sciences and Research, Mullana, District - Ambala, Haryana, and other departments of MM College of Medical Sciences, Mullana, District - Ambala, Haryana, including the emergency. Comminuted, grossly displaced and dentoalveolar fractures were not included in the study. In our study 2.0 mm diameter, 12 mm long transalveolar self-tapping titanium screws were used. These screws were placed in maxilla and mandible (Figure 2). In 9 out of the 10 patients two screws per arch were placed while in one patient three screws per arch were placed, strategically so as to avoid root apices or neurovascular bundle. Arthur and Berardo[5] in 1989 first suggested the use of 2 mm self tapping screws to secure MMF, but Busch[6],[7].[8].[10],[16] advocated the use of 2.7 mm self tapping screws as the 2 mm screws were thought to be brittle. Gordon et al[9] also supported the use of 2.7 mm self tapping screws, but Jones[8],[12], Glickman[11], Thotha[13], Ueki[14], Schneider[15], Gibbons[17],[19] and Vartanian[18] all favored the use of 2 mm self tapping screws. Follow up visits were planned at 7 days, 15 days, 1 month, 2 months, 3 months and 5 months from the day of removal of the MMF apparatus. Breach of glove barrier was deemed as one of the main parameters since transalveolar screws were developed with the main aim to lower the risk of the operator when working on a HIV positive patient or a HBV positive patient.
 | Fig 2: Profile View
 |
 | Fig 2: Pre Operative Occlusion
 |
 | Fig 2: Pre Operative Right Side
 |
 | Fig 2: Pre Operative Left Side
 |
 | Fig 2: Pre Operative Orthopantomogram Showing A Fracture Of The Right Subcondyle And Left Angle Of The Mandible.
 |
 | Fig 2: Intra Operative Occlusion
 |
 | Fig 2: Intra Operative Right Side
 |
 | Fig 2: Intra Operative Left Side
 |
 | Fig 2: Intra Operative Orthopantomogram.
 |
 | Fig 2: Post Operative Occlusion
 |
 | Fig 2: Post Operative Right Side
 |
 | Fig 2: Post Operative Left Side
 |
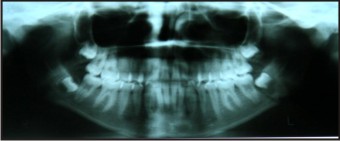 | Fig 2: Post Operative Orthopantomogram
 |
1 screw fracture was seen during the entire study which was in the 32, 33 region. The screw was left in place and an alternative site was prepared for screw fixation inferior to the site of screw fracture. The fractured screw was checked radiographically in the follow up visits. In the studies by Coburn[20] 3 screw fractures were seen in 122 patients and the screws were left in place uneventfully, Salama et al[22] report 4% screw fractures, Molina et al[23] report 4 cases of screw fracture in 60 patients while Coletti et al[24] report 2 (4%) cases of screw fracture in 49 patients. The time required for application of apparatus as well as for the removal of apparatus is very less and the whole process is also more comfortable for the patient. This method also has a good patient compliance with no swelling or bleeding noted from the site of MMF application. The main advantage also noted in our study is of minimal glove perforation. The high cost and its limitation in cases with displaced and comminuted fractures is a major drawback. All the disadvantages of transalveolar screws along with the tendency of the screws to become loose and unstable after a few days of application caused severe pain and discomfort to the patient. Also it was noted that of the 42 screws applied 1 fractured on application while 9 screws were covered by mucosa (Figure 3). In the reviewed literature by Jones[8],[12], Glickman[11], Thotha[13], Ueki[14], Schneider[15], Gibbons[17],[19], Vartanian[18], Roccia et al[21], Salama[22], Molina et al[23] and Coletti et al[24] it was noted that these screws have a great tendency to cause iatrogenic tooth injury which however was not seen in our study.
 | Fig 3: Complications Of Transalveolar Screws
 |
References
1. History of maxillofacial trauma, Norman Lester Rowe, Annals of Royal College of Surgery, 1971, Vol. 49, PP 329 – 349.
2. Kurt H. Thoma, Treatment of jaw fractures past and present, Journal Of Oral Surgery, 1959, PP 30 – 47.
3. Hashmi S.H., Chawla T.N., Pradhan R., Sharma V.D., An analysis of maxillofacial injuries, Journal of Indian Dental Association, 1980, Vol. 52, PP 219 – 220.
4. S.Lida, M.Kogo, T.Sugiura, T.Mima, T.Matsayu, Retrospective analysis of 1502 patients with facial fractures, International Journal of Oral and Maxillofacial Surgery, 2001, Vol. 30, PP 286 – 290.
5. Arthur Gregory and Bernando Nicholas, A simplified technique of Maxillomandibular Fixation, Journal Of Oral Maxillofacial Surgery-1989, Vol. 47, p 1234.
6. Busch Richard F. & Prunes Fernando, Intermaxillary Fixation with Intraoral Cortical Bone Screws, Laryngoscope- 1991, Vol.101, pp 1336-1338.
7. K.K.S. Win, Y. Handa, H. Ichihara, N. Tatematsu, H. Fujitsuka and T. Ohkubo, Intermaxillary fixation using screws, International Journal of Oral Maxillofacial Surgery, 1991, Vol. 20, PP 283 – 284.
8. D Carl Jones, Letter to the Editor, Oral Surgery Oral Medicine Oral Pathology, 1997, No. 85, Vol. 5, PP 458 – 459.
9. Gordon Kyle.F., Reed Mark.J. and Anand Vinod.K., Results of intraoral cortical bone screw fixation technique for mandibular fractures, Otolaryngology- Head and Neck Surgery- 1995, Vol. 113, No. 3, pp 248-252.
10. Busch Richard.F, Mandibular osteosynthesis with intraoral miniplates & cortical bone screws, ENT- Ear, Nose and Throat Journal- 1995, Vol. 74, No. 12, pp 817-820.
11. Valsiki Karlis and Robert Glickman, An alternative to arch bar maxillomandibular fixation, Plastic Reconstructive Surgery, 1997, Vol. 99, PP 1758 – 1759.
12. D.C.Jones, The intermaxillary screw: A dedicated bicortical bone screw for temporary intermaxillary fixation, British Journal of Oral and Maxillofacial Surgery, 1999, Vol. 37, PP 115 – 116.
13. L.G. Thotha and D.A. Mithchell, Cortical bone screws for maxillomandibular fixation in orthognathic surgery, Journal of Orthodontics, 1999, Vol. 26, PP 325 – 326.
14. Koichero Ueki, Kohei Maruwaka, Mayumi Shimada, Kiyomasa Nakagawa and Estubide Yamamoto, The use of an Intermaxillary fixation screw for mandibular setback surgery, Journal of Oral Maxillofacial Surgery, 2007, Vol. 65, PP 1562 – 1568.
15. Andrew M.Schneider, Lisa R.David, Anthony J.Defranzo, Use of specialized bone screws for intermaxillary fixation, Annals of Plastic Surgery, 2000, Vol. 44, PP 154 – 157.
16. R.F. Busch, Re: Jones, Intermaxillary fixation using intraoral cortical bone screws, British Journal of Oral and Maxillofacial Surgery, 2000, Vol. 37, P 422.
17. A.J. Gibbons and S.C. Hodder, A self drilling intermaxillary fixation screw, British Journal of Oral and Maxillofacial Surgery, 2003, Vol. 41, PP 48 – 49.
18. A. John Vartanian and Aijaz Alvi, Bone screw mandible fixation: An intraoperative alternative to arch bars, Otolaryngology Head Neck Surgery, 2000, Vol. 123, PP 718 – 721.
19. Andrew J. Gibbons, Self drilling intermaxillary fixation screws in the closed treatment of a condylar fracture, Journal of Oral Maxillofacial Surgery, 2007, Vol. 65, P 357.
20. Coburn D.G., Kennedy D.W.G. & Hodder S.C., Complications with intermaxillary fixation screws in the management of fractured mandibles, British Journal of Oral and Maxillofacial Surgery- 2002, Vol. 40, pp 241-243.
21. Fabio Roccia, Amedeo Tavolaccini, Alessandro Dell’Acqua and Massimo Fasolis, An audit of mandibular fractures treated by intermaxillary fixation using intraoral cortical bone screws, Journal of Cranio – Maxillofacial Surgery, 2005, Vol. 33, PP 251 – 254.
22. Andrew Salama, Application of IMF screws in maxillofacial trauma: A pilot study to examine efficacy & safety, Journal of Oral & Maxillofacial Surgery, 2005, Vol. 63, PP 60 – 61.
23. J. Molina, J. Mareque, J.A. Hueto, J. Gonzales- Lagunas and G. Raspall, Dental damage with intermaxillary fixation screws in the treatment of mandibular fractures, Journal of Cranio- Maxillofacial Surgery, 2006, Vol. 34, P 88.
24. Domenick P.Coletti, Andrew Salama, John F.Caccamese, Application of intermaxillary fixation screws in maxillofacial trauma, Journal of Oral Maxillofacial Surgery2007, Vol. 65, PP 1746 – 1750.
|